To download the pdf of the presentation, click here.
To register for the next webinar in our series, please click here.
Presenter Joanna Scott-Lutyens has kindly answered the following questions, which were asked during the webinar:
Aren’t all probiotics transient and not meant to colonise but do all the good re terrain whilst they are there? If bacteria are found live in the stool does this mean that they do actually repopulate the gut or does it mean they are transient?
Some probiotics are transient, and others are colonising because they can adhere to the gut lining. Probiotics such as some found in kefir cultures, or indeed Saccharomyces boulardii are transient, yet still classified as probiotics. However, for gut bacteria to repopulate, they need to adhere to the gut wall. When trying to rebalance our healthy bacteria, we want to be growing these in numbers, therefore they need to adhere and repopulate. Having said that pretty much all probiotics would end up leaving the gut after a certain period of time, such as a few weeks. Both transient and colonising bacteria are necessary for gut health but colonising bacteria are considered to be the gold standard for making changes in the gut which is why I would advocate a healthy diet with prebiotics and probiotic foods alongside a quality probiotic for addressing gut health.
What book/info about probiotic strains related to symptoms?
I assume you are asking for the title of the book I mentioned in my webinar? It’s Yuan Kun Lee et al. (2009) Handbook of Probiotics and Prebiotics, 2nd Edition Wiley: New Jersey
However, company websites should have information about their products and links to research literature where you can find out what research is behind a strain and indeed what that research has been looking into in terms of symptoms. Optibac Probiotics has a research section on the website which you might find interesting. https://www.optibacprobiotics.co.uk/scientific-research
When recommending probiotics alongside antibiotics a client is taking, is it crucial to distinguish between strains? Or can we recommend any probiotic strain?
Yes the strain is relevant. It’s important to find the strains that have research behind them showing not only that they have survived antibiotics but also that they help prevent AAD (Antibiotic Associated Diarrhoea). As mentioned in the webinar two strains that have shown this are Lactobacillus rhamnosus Rosell-11, Lactobacillus acidophilus Rosell-52 which can be found in our ‘For those on Antibiotics’ product. These have a lot of research behind them showing that they reduce the incidence of AAD but also have been tested against multiple types of antibiotics
When dealing with histamine intolerances, how do respond based on the bacteria having been cultured. Also what strain would be ideal if so.
I believe you are asking if the fermentation process that happens to produce probiotics, produce a histamine containing probiotic? Probiotic supplements shouldn’t contain histamine given that the bacteria are isolated from its growth medium and purified before encapsulated. We also know that good levels of friendly bacteria may contribute to lower fermentation of protein in the gut which may lead to the production of histamine from histidine. There is some research on which strains are thought to be particularly beneficial for histamine intolerances and others that are thought to aggravate the situation. However, this research is very inconclusive, and a lot more is required before we can know much more. You can find more information on this on our website in the FAQ on probiotic for histamine intolerance https://www.optibacprobiotics.co.uk/faq/which-probiotic-for-histamine-intolerance
Thank you for the presentation! Would you recommend to change brands of probiotics manufactures often? Thank you..Yelena.
Hello Yelena. I’m glad you liked the presentation. I think it is important to find the right probiotic product with the right strain for your, or your client’s symptoms. If you find a product that works, then there is no need to change manufacturers. I would just say that it can sometimes take a couple of goes to find the right one for you. I would suggest you identify the primary symptom you would like to address, and then find a probiotic supplement that addresses that symptom/ issue – just remember to check for whole strain name on packet, availability of research etc. If you need more information on our products or have a specific question please do not hesitate to contact me.
Please repeat the name of the book (probiotics). Thank you.
It’s Yuan Kun Lee et al. (2009) Handbook of Probiotics and Prebiotics, 2nd Edition Wiley: New Jersey. Thank you
What do you recommend for baby?
If the baby is new born it is important to choose a product that is designed for that age group. These usually come in sachet format for easy mixing with milk or water as well. OptiBac Probiotics ‘For babies and children’ contains strains that are known to be found in a new-born’s gut and can be taken from birth and also by the mother when pregnant or breast feeding. However, if the baby is suffering from other issues such as constipation, diarrhoea etc., a more specific probiotic product might be applicable. However, these are usually ok for a baby to take from 1 year up so do check with the company. Please see our FAQ on probiotics for children for our products here https://www.optibacprobiotics.co.uk/faq/are-optibac-probiotics-suitable-for-children
Do you know a good product containing L Plantarum 299V, as I have a client with long term anaemia?
I’m sorry but we do not have this particular strain of L. plantarum. We have two different strains from this species but these are used for cholesterol control. I believe you can buy this from Solgar. The product is called Probi and is available in the UK at 20bn or 30bn strengths.
What about prebiotics has an influence on microbiome? This includes the ones included in the symbiotic formulation
Prebiotics are a source of food for probiotics to grow, multiply and survive in the gut. Research shows that there are different types of prebiotics, in a similar manner as there are different types of probiotics. With prebiotics, the key differentiating factor is the length of the chemical chain – short chain; medium chain or long chain determines where in the gastrointestinal tract the prebiotic has its effect, and how the benefits may be felt by the host. Common prebiotics include: inulin, fructooligosaccharides (FOS), galactooligosaccharides (GOS), and lactulose. Within the OptiBac Probiotics range, the prebiotic FOS can be found in ‘For every day‘, ‘One week flat‘, ‘For babies HYPERLINK “https://www.optibacprobiotics.co.uk/shop/for-babies-children”& HYPERLINK “https://www.optibacprobiotics.co.uk/shop/for-babies-children” children‘ and ‘Bifidobacteria & fibre‘. Two key properties of the FOS found in these products, which have an influence on the microbiome are: indigestibility in the small intestine, and fermentability in the colon. They are converted into short chain fatty acids (SCFAs) by intestinal bacteria, and these SCFAs largely feed the colonocytes and have numerous health promoting effects. They improve the gut mucosal barrier and modulate microflora diversity, they improve the absorption of several minerals including calcium and magnesium and they enhance the immune system to name a few!
Why does taking probiotics sometimes cause stomach upset?
Temporary reactions such as minor bloating or a mild laxative or constipating effect are signs that the beneficial bacteria are remodelling, detoxifying and improving the gut environment. Assuming any adverse effect is relatively minor and does not persist for more than 2 weeks, this response is not unusual, and it is important to give your body some time to adjust. In the case of any persisting side effects, I would recommend decreasing the dose or trying a different formulation.
Another thing to bear in mind is that some probiotic products may contain a prebiotic in their formulation. Common prebiotics include: inulin, Fructooligosaccharides (FOS) and galactooligosaccharides (GOS). The prebiotic is added to aid the colonisation of the probiotics. In some cases however, prebiotics can cause minor disturbances/ flatulence in the first few days of taking then, but after 3-4 days of continued use, (once the intestines have adapted to the prebiotics) this discomfort tends to disappear.
Is there a list that we could have, of well investigated strains with reference to improving specific conditions?Is there a resource where we can look up which strain can be matched with the particular symptoms
At the moment unfortunately there isn’t a resource like this. It really is a case of googling this and then ascertaining whether the products you come up with are quality and from a reputable company. I appreciate this is quite time consuming and not ideal. Also remember that unless addressing a particular symptom, we are sometime trying to heal the gut in order to address a symptom – allergies being a good example of this. So in some cases probiotic strains have been researched for allergy. But also we know that addressing gut health and improving gut integrity is vital here. In answer to your question, the best that I can do at the moment is to direct you to the scientific research page on our website as well as provide the database of clinical trials on our finished products and strains in our range – see attached. I hope you find these resources helpful!
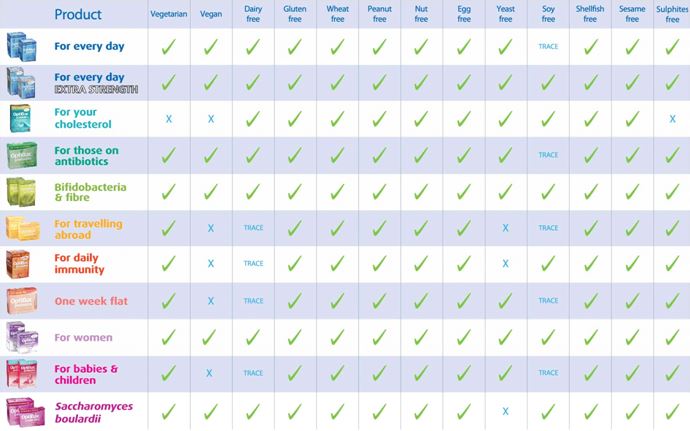
Are there allergy free probiotic supplements?
Yes, allergy free probiotics in terms of dairy free, gluten free and vegan etc. do exist, and will be stated on the external packaging of any reputable probiotic. In terms of the OptiBac Probiotics range the table below outlines the allergy information regarding our products:
Is there a difference between “human based” probiotic and non-human based probiotic?
The term “human based” refers to probiotic strains, which were originally isolated from the human body as opposed to other sources such as dairy or fruit. The difference here lies in the fact that these strains of bacteria would typically be found as a natural resident of a healthy human gut as oppose to an externally derived microorganism. It is however important to remember, that we are surrounded by a plethora of bacteria in the environment, and an influx through the foods we consume which can also make it to the gut, where they may reside and have physiological effects. So to distinguish probiotic strains on their source is not particularly relevant. What can be said here however, is that human strains tend to come from human faeces, and this acts as evidence for their capability to survive intestinal transit – a key factor when considering a good probiotic. That being said, there is no existing evidence that human strains are more capable of adhering to, or colonizing the human gut than no human strains.
Therefore what is key when considering differences between probiotics is not their source, but identifying whether they have been verified and tested to colonies their target site, and furthermore to look to their strain names to differentiate their mode of action.
Once a pot of probiotic has been taken (over, say 4 weeks), how soon will a stool sample return to the pre-treatment profile?
Well this really depends on a number of factors, but predominantly it depends on the individual and their lifestyle, so to give a definitive answer to your question is near impossible. Gut profiles are constantly undergoing change. What can be said, is that there are many, many factors that can negatively affect the probiotic colonies in our gut, and so we really must nurture it on an ongoing basis. To support the colonies that inhabit the gut as a result of probiotic treatment, a diet rich in fibre and fresh, organic fruits and vegetables is a good starting point. To slow the decline, which is equally important, trying to avoid factors that may negatively affect the probiotic colonies is key. For example, reducing our exposure to the low level of antibiotics that we can be exposed to through the food chain in non-organic meat and dairy produce. Chemicals like chlorine in our drinking water are potent anti-microbial agents that may damage our delicate gut flora, over consumption on sugar, the contraceptive pill, HRT medication and stress all have a negative impact, and the list goes on! With all of these things in mind, while probiotic treatment can be excellent for certain conditions at perhaps more potent doses, it is easy to see here why a daily top-up of probiotics would be a good idea following treatment to maintain a microbial diversity in our gut and stool sample.
Is it necessary to take probiotic supplements daily and permanently?
Many people choose to take probiotics every day, whilst some might just use them periodically or whenever they feel that their digestive health needs a boost. Whichever way you find works best for you or your clients, it is worth remembering that many factors can negatively affect the probiotic colonies in our gut. Our lifestyles are now so challenging for our microbiome that many of us need to nurture it on an ongoing basis.
As you may know, antibiotics do not differentiate between the good and bad bacteria in our guts, and therefore negatively impact on our probiotic colonies, but we often do not look at all the different sources of antibiotics in our food chain. Not only are we exposed to antibiotics when we take them ourselves, but we are exposed to low levels all the time if we eat non-organic meat and dairy produce. These have a similarly negative impact on our gut flora.
In addition, we are often exposed to chemicals such as chlorine in our drinking water. Chlorine is a strong anti-microbial agent, and whilst it helps to keep undesirable bacteria out of our water supply, it also damages our delicate gut flora.
Other factors that deplete our flora include, over-consumption of sugar, contraceptive pills, HRT medication and stress. With all of these things considered, a daily top-up of probiotics would be a good idea for many people. Like most vitamins and minerals, we do not produce probiotics ourselves, so we need an external source of them.
Is there any advice on whether to take a probiotic with/without food? Avoiding hot drinks?
An important factor in a high quality probiotic is its ability to survive through gastric acidity. If a probiotic has not been tested to survive gastric acidity and biliary salts then it may not reach the intestine, which is where it needs to settle in order to exert its beneficial effects on the body. Research from microbiologists’ shows that at mealtimes (and especially breakfast time) the stomach’s gastric acidity is naturally at its least acidic. So when recommending when to take a probiotics, it is suggested to be taken with a meal, ideally breakfast; this is when the probiotics will have the optimum survival rate through the body’s gastric acidity.
In terms of hot drinks, it is true that heat kills bacteria so you may not want to literally put your probiotics (in the case of a sachet) in a hot drink. However we don’t tend to worry too much about taking probiotics with a hot drink because by the time it is cool enough to drink, its closer to body temperature – which the probiotics will be subjected to anyway. If you would prefer to err on the side of caution, I would recommend taking your probiotic capsule or sachet with a cold drink, then sipping hot drink afterwards.
How are probiotics made?
This varies from product to product of course. However, typically probiotic supplements are made this way: The bacterial strains chosen are grown and fermented on a medium typically dairy or soya. This is left to ferment and grow and is then centrifuged which is where a machine spins it at top speed separating the bacteria from the food molecules. The bacteria are then freeze dried to evaporate any remaining water and put in a dormant state. All of this is done under very tightly controlled conditions in a lab, and then packed so that no oxygen or moisture can contact the bacteria. This creates a bacteria with a high degree of purity.
How are the various strains cultured? On what substrate?
This varies from product to product. Please do contact us for further details.
Can I take the product out of the capsule?
Yes you can. This ties in nicely with the discussion about enteric coating not being necessary and that the quality of the strain is important – we get asked this a lot as not everyone can take a capsule easily so we suggest that you open the capsule and add it to your food or on in a yogurt. I would just recommend that you don’t leave the powder open to the air in food prepared and then left for ages as the O2 could degrade the bacteria.
You talk about strains needing to be good quality and therefore the strength not being important – are you saying that it’s never important to have a strong good quality probiotic?
No, this is not the case. Sometimes a low dose of a particular bacterial strain is all that is required to alleviate a particular symptom (such as in the BB-12 constipation study) so there is no need to use a higher strength one. However, there are of course cases where a stronger dose of probiotic may be beneficial. Sometimes we can use the length of time that person has been unwell for, how severe the symptoms are as a guide. So for example with extreme diarrhoea or candida the dose suggested of SB would be more than the amount that is in the travel product which is a more precautionary / protective dose. It’s always unique to that person and their symptoms.
